Factors associated with within-individual variability of lung function for people with cystic fibrosis: a longitudinal registry study
Abstract
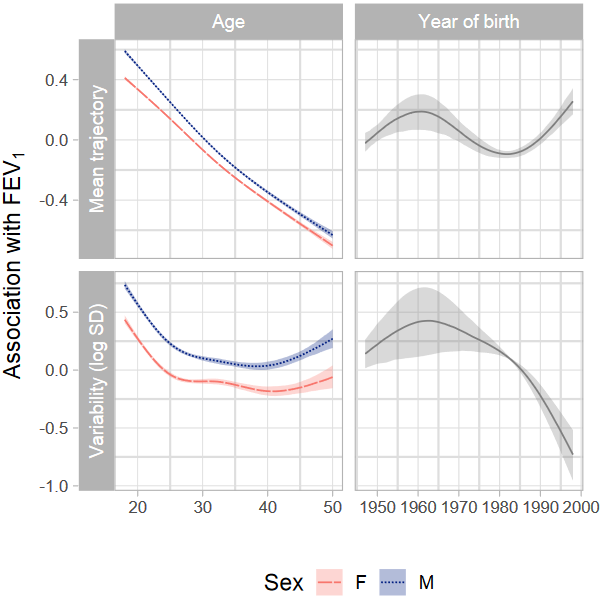
Lung function is a key outcome used in the evaluation of disease progression in cystic fibrosis. The variability of individual lung function measurements over time (within-individual variability) has been shown to predict subsequent lung function changes. Nevertheless, the association between within-individual lung function variability and demographic and genetic covariates is not quantified. We performed a longitudinal analysis of data from a cohort of 7099 adults with cystic fibrosis (between 18 and 49 years old) from the UK cystic fibrosis registry, containing annual review data between 1996 and 2020. A mixed-effects location-scale model is used to quantify mean FEV1 (forced expiratory volume in 1 second) trajectories and FEV1 within-individual variability as a function of sex, age at annual review, age at diagnosis, genotype and birth cohort. Mean FEV1 decreased with age and lung function variability showed an approximately quadratic trend by age. Males showed higher FEV1 mean and variability than females across the whole age range. Individuals who died during follow-up showed on average higher lung function variability than those who survived. This work opens new avenues for further research to understand the role of within-individual lung function variability in disease progression and prediction of key outcomes such as mortality.